Orthopedic Oncology
Advanced Bone & Soft-Tissue Tumor Care —Limb-Salvage, Precision Reconstruction, Optimal Function.
Multidisciplinary sarcoma management, custom 3-D implants, and metastatic bone disease expertise.
We provide comprehensive musculoskeletal oncologic care—from image-guided biopsy and multidisciplinary tumor-board planning to complex resection, microvascular reconstruction, endoprosthetic or allograft reconstruction, and adjuvant therapy coordination. Advanced navigation, intra-operative imaging, and patient-specific 3-D guides ensure maximal tumor clearance with optimal function. Dedicated metastatic-bone-disease pathways integrate interventional radiology ablation, cementoplasty, and targeted systemic therapy.
> 380
bone & soft-tissue tumor cases treated in 202492%
limb-salvage rate for extremity sarcomas<2 weeks
custom 3-D printed implants (design to OR)Same-day
virtual second-opinion for outside pathology/imagingCommon Conditions & Subspecialty Clinics.
- Age-adapted chemotherapy regimens
- Expandable growing endoprostheses for limb preservation
- Combined damage-control orthopedics and oncologic alignment management
- Custom 3D-printed endoprostheses
- Allograft–prosthetic composites
- Rotationplasty for pediatric limb tumors
- Osteoid osteoma – radiofrequency ablation (RFA)
- Diagnosis and treatment of a wide range of eye conditions
- Desmoid tumor – conservative and medical therapy
- Pathologic fracture fixation
- Prophylactic intramedullary nailing
- Cementoplasty
- Planning for stereotactic body radiotherapy (SBRT)
- Liposarcoma
- Synovial sarcoma
- Undifferentiated pleomorphic sarcoma
- Wide local excision with negative margins and soft-tissue reconstruction
- Osteosarcoma
- Ewing sarcoma
- Chondrosarcoma
- Adamantinoma
- Neoadjuvant chemotherapy coordination and limb-salvage surgery
Procedures & Treatments.
Molecular pathology (MDM2, EWSR1, SS18 translocations) for subtype confirmation
Angiography/embolization for hypervascular tumors pre-resection
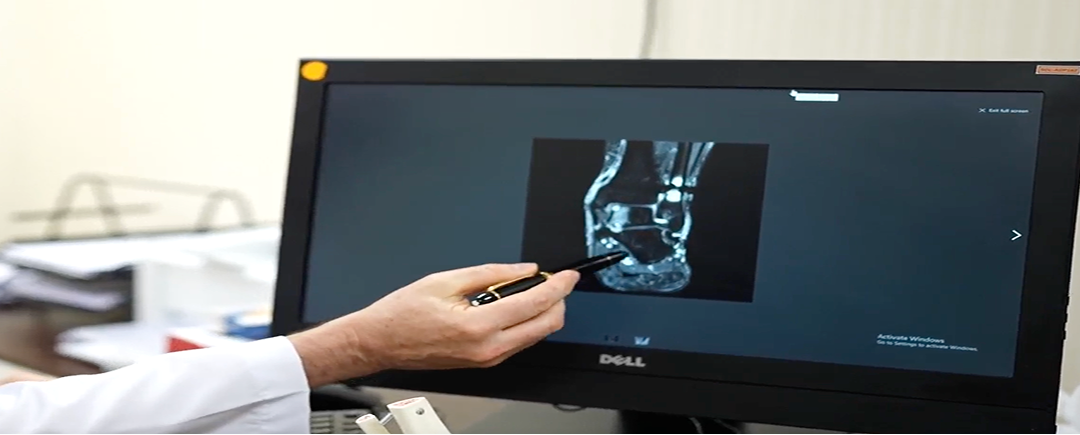
High-resolution CT for cortical involvement and 3-D planning
CT-guided core biopsy with on-site pathologist adequacy check
Whole-body MRI and ¹⁸F-FDG PET-CT for metastasis assessment
Pathologic Fracture Fixation—locking plates, intramedullary nails, modular stems
Microvascular Free-Flap Soft-Tissue Coverage—ALT, latissimus, fibula
Rotationplasty as function-preserving alternative to amputation
Expandable Pediatric Endoprosthesis allowing growth without repeat surgery
Allograft-Prosthetic Composite Reconstruction for joint preservation
3-D-Printed Titanium Endoprostheses—pelvic, scapular, and long-bone replacements
Computer-Navigated Tumor Resection with patient-specific cutting guides
Bisphosphonate or RANK-Ligand inhibitor for skeletal-related-event prevention
Denosumab for giant-cell tumor and bone-metastasis stabilization
Radiofrequency/microwave ablation + cementoplasty for painful metastases
IMRT/VMAT & SBRT for margin boost or unresectable lesions
Neo-adjuvant & adjuvant chemotherapy per EURAMOS/COG protocols
Psychosocial support and vocational reintegration services
Cancer-rehab program—strength, gait training, lymphedema management
Advanced prosthetics-and-orthotics lab for custom bracing/limb devices
Early weight-bearing protocols with physiotherapy
Care Pathway & Coordination.
Rapid Referral & Imaging Review
Pathology & imaging reviewed within 48 h; core biopsy scheduled.
Sarcoma Tumor Board
Multidisciplinary plan: surgery, chemo, RT.
Pre-op Planning
3-D modeling, implant design, tissue-flap selection.
Definitive Surgery / Procedure
Limb-salvage resection & reconstruction.
Post-Op & Adjuvant Therapy
Chemotherapy / RT as per protocol; rehab initiation Day
Long-Term Surveillance
Imaging at 3-6-month intervals; survivorship clinic for prosthesis monitoring.
Technology & Facilities.
CT-Based 3-D Printing Lab
Patient-specific cutting guides and implants
Intra-operative Navigation & Augmented Reality for margin accuracy
Hybrid OR with Cone-Beam CT
Real-time imaging during resection
Modular Endoprosthesis Inventory
Immediate off-the-shelf options
Multi-axis Isokinetic Strength Testing
Functional outcome tracking
Gait-Analysis Lab
Motion capture to optimize rehabilitation
